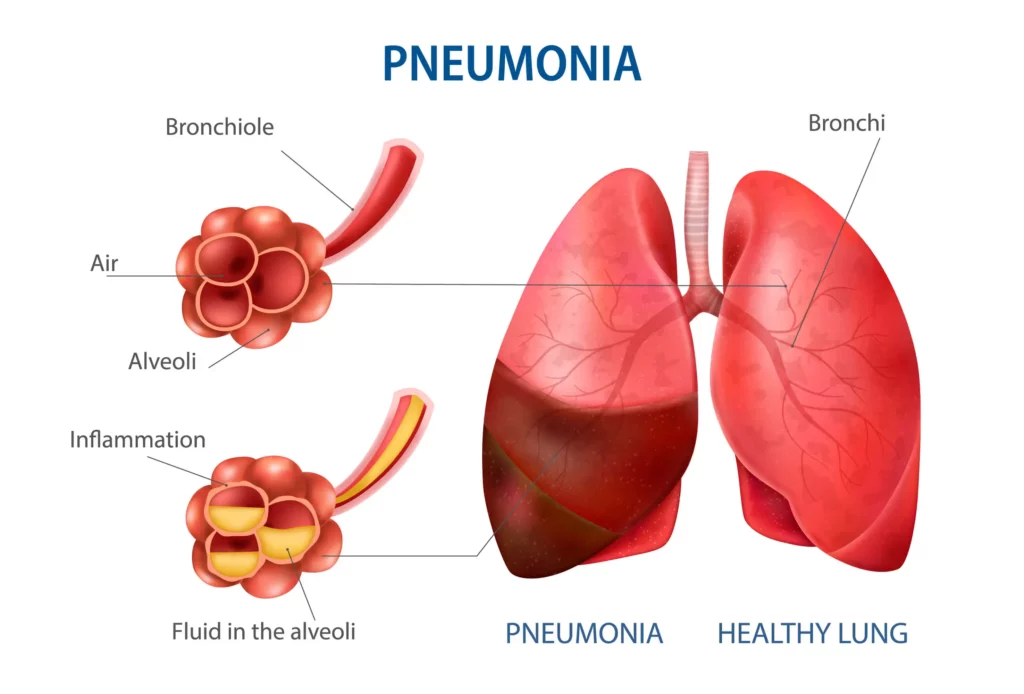
Pneumonia is an inflammatory condition of the lungs following any bacterial, viral, or fungal infection. Our lungs consist of small air sac-like structures called alveoli. These alveoli get filled with fluid or pus, which leads to the consolidation of the lungs. Hence due to consolidation, the individual finds it difficult to breathe.
Pneumonia is a contagious disease that can transmit from one person to another through inhalation of airborne droplets from a sneeze or cough. Also, one can get affected by coming into contact with surfaces or objects contaminated with pneumonia-causing bacteria or viruses.
WHAT ARE THE CAUSES OF PNEUMONIA?
Pneumonia occurs when your lungs get infected by germs. The immune system’s reaction to eradicate the infection results in inflammation of the lung’s air sacs. This inflammation can eventually cause the air sacs to fill with pus and fluids, causing pneumonia.
Many bacteria, viruses, and fungi are responsible for pneumonia. Bacteria are the most common cause in adults, and viruses are the most common cause in school-going children.
TYPES OF PNEUMONIA
Based on how pneumonia is acquired, it is classified into four types:
* Community-acquired pneumonia (CAP) refers to pneumonia acquired outside a medical center.
* Hospital-acquired pneumonia (HAP) is bacterial pneumonia acquired in a hospital due to some illness or procedure. It can be more serious than other types, as it is caused by antibiotic-resistant bacteria, which can be difficult to treat.
* Ventilator-associated pneumonia (VAP). You are more likely to get infected by this pneumonia when bedridden and require a breathing machine (in ICU).
* Aspiration pneumonia. Inhaling bacteria into your lungs from food, drink, or saliva can cause aspiration pneumonia.
WHAT ARE THE SIGNS AND SYMPTOMS OF PNEUMONIA?
The onset and the appearance of the symptoms vary from person to person, depending upon their age and general health condition. It can range from mild symptoms like coughing to life-threatening conditions like sepsis, pleural effusion, etc.
- An individual may experience any of the below-mentioned symptoms:
- A high fever (>39 degrees celsius) will accompany chills and rigors.
- Sudden onset of cough along with yellow/green or blood-stained mucus.
- The person feels shortness of breath while performing any activity or resting.
- Chest pain which alleviates while coughing.
- There is an increased respiratory rate and heart rate.
- Tiredness(fatigue)
- Gradual loss of appetite
- Bluish color of skin and nail beds(cyanosis)
- Headaches and muscle pain are also common.
Other symptoms can vary according to your age and general health:
- Infants may appear to have no symptoms, but sometimes they may vomit, lack energy, and resist drinking or eating.
- Children under 5 years old may have fast breathing or wheezing. They face difficulty while sleeping.
- Older adults may have milder symptoms. They can also experience confusion or a lower-than-normal body temperature.
WHO IS AT A POTENTIALLY HIGHER RISK OF DEVELOPING PNEUMONIA?
Individuals who are at a higher risk of developing pneumonia are :
- Individuals above 65 are more prone to pneumonia because their capacity to fight the disease decreases as age advances.
- It is more common in immunocompromised individuals who have poor immune systems. Such individuals possess poor defense mechanisms to deal with harmful substances entering the body. E.g.:
- pregnancy
- HIV
- the use of certain medications, such as steroids or certain cancer drugs
- Infants from birth to 2 years of age.
- People suffer from chronic conditions like asthma, COPD, diabetes, heart failure, and liver diseases.
- People who’ve been hospitalized for a long duration. Most importantly, if they are on a ventilator.
- Patients suffering from neurological problems like Parkinson’s disease, dementia, etc. These ailments affect the patient’s ability to swallow properly.
- People who smoke are more likely to develop pneumonia as smoke damages the cilia in air passages. These cilia are responsible for clearing up mucus.
HOW TO DIAGNOSE PNEUMONIA?
Your doctor will commence by taking your medical history. They will then examine you physically. This will include listening to your lungs with a stethoscope for abnormal sounds, such as crackling. Depending on the clinical presentation of your symptoms and your general health condition, your doctor may suggest certain investigations:
Chest X-ray
An X-ray helps your doctor look for signs of inflammation and consolidation in your chest. Consolidated areas look opaque in the x-ray. The location and extent of the lesion can also be determined.
Blood culture
This test uses a blood sample to confirm an infection.
Sputum culture
During a sputum culture, a mucus sample is collected using a swab. It is then examined to inspect the cause of infection.
Pulse oximetry
Pulse oximetry measures the amount of oxygen in your arterial blood. It can indicate whether your lungs are moving enough oxygen through your bloodstream.
CT scan
CT scans provide a clearer and more detailed picture of your lungs.
Bronchoscopy
A flexible tube-like device is gently guided down your throat and into your lungs in bronchoscopy. This is attached with a camera at the end, which gives you a whole view of the lungs. Your doctor may do this test if your initial symptoms are severe.
WHAT IS THE TREATMENT PROTOCOL FOR PNEUMONIA?
Your treatment will depend on your type of pneumonia, how severe it is, and your general health.
Drug therapy
It includes a course of antibiotics that are used to eliminate the infection. What you are prescribed will depend on the specific cause of your pneumonia. Oral antibiotics can treat most cases of bacterial pneumonia. Antibiotic medications don’t work on viruses.
Viral pneumonia usually isn’t treated with medication and can go away alone. In some cases, your doctor may prescribe an antiviral medicine. E.g., acyclovir, peramivir, etc. Similarly, in cases of fungal infections, antifungal medication is prescribed.
Oxygen therapy:
Your doctor might switch to oxygen therapy if you’re not getting enough oxygen. Here supplemental oxygen is supplied via a tube attached to a cannula (nose mask). This therapy is given in critical cases where the patient is severely affected.
IV fluids:
Fluids are delivered directly through your vein to prevent dehydration.
Draining of fluids:
If you have a lot of fluid between your lungs and chest wall (pleural effusion), a provider may drain it. This is done with a catheter or surgery.
WHY DOCTOR NARANG?
Dr. Rajeev Narang is a well-known pulmonology doctor in Jaipur. He deals with all respiratory disease patients with over 18 Years of a wonderful experience. He deals with the individual one-to-one and formulates the treatment plan by thoroughly investigating the patient’s clinical conditions and giving the best medical treatment possible. Dr. Rajeev Narang is one of the best pulmonology doctors in Jaipur you can consult.